Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum. Characterized by inflammation and ulceration of the innermost lining of the large intestine, UC can lead to severe symptoms such as diarrhea, abdominal pain, fatigue, weight loss, and rectal bleeding. Ulcerative Colitis Epidemiology Analysis While the exact cause remains unknown, genetic, environmental, and immune factors contribute to the development of the disease.
This article provides an epidemiological analysis of ulcerative colitis, highlighting its global prevalence, incidence, risk factors, and the burden of the disease on healthcare systems worldwide.
1. Global Prevalence and Incidence of Ulcerative Colitis
The prevalence and incidence of ulcerative colitis vary significantly across different regions, with the highest rates typically reported in Western countries, particularly in North America and Europe. However, the disease is increasingly recognized as a global health concern, with rising rates of diagnosis in developing regions, especially in Asia, the Middle East, and South America.
Prevalence in North America and Europe
Ulcerative colitis is most commonly diagnosed in high-income, industrialized countries, particularly in North America and Europe. Estimates suggest that in the United States, the prevalence of UC ranges from 37 to 246 cases per 100,000 individuals, with approximately 750,000 Americans living with the disease. In Canada, the prevalence is similarly high, with an estimated 233 cases per 100,000 people.
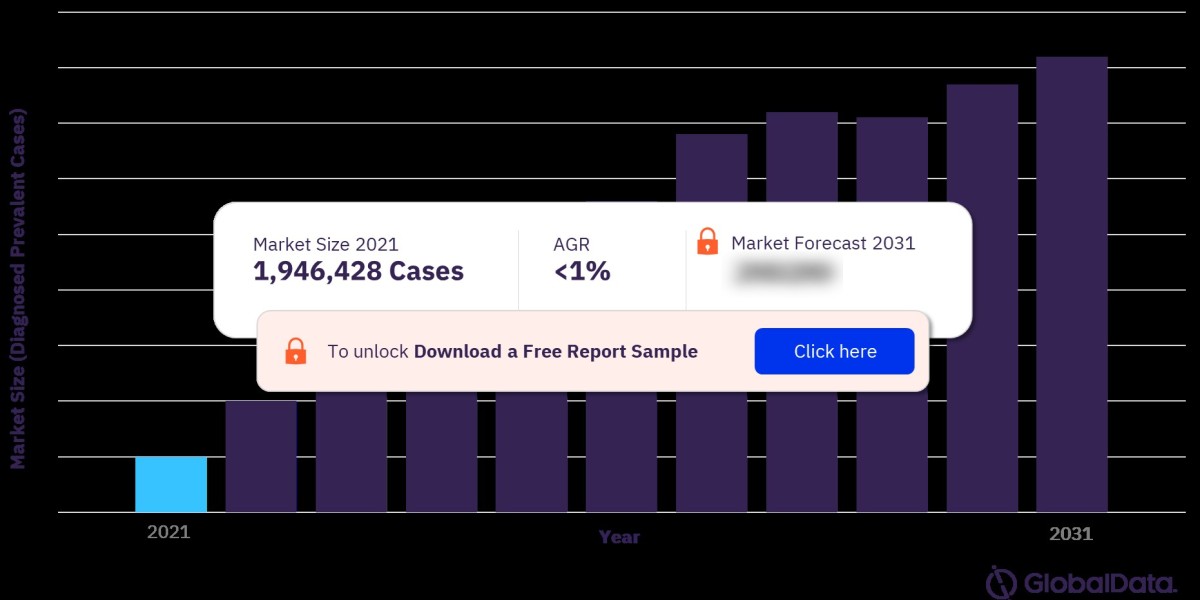
In Europe, the prevalence rates vary widely across countries, but it is generally reported to be between 50 and 250 cases per 100,000 individuals. The United Kingdom, Scandinavia, and northern European countries have some of the highest prevalence rates, while southern and eastern European countries report lower rates of UC. For more insights into the Ulcerative Colitis market forecast, download a free report sample
Emerging Incidence in Asia and the Middle East
Historically, ulcerative colitis was considered rare in Asia, the Middle East, and Africa. However, in recent years, the incidence of UC has been increasing in these regions, likely due to changing lifestyles, dietary patterns, and urbanization. In countries like Japan, China, and India, the incidence of UC is rising rapidly, with incidence rates now estimated to be between 5 and 25 per 100,000 individuals in these regions.
This increase is also observed in Middle Eastern countries, where the incidence and prevalence of UC are rising as the region undergoes rapid socioeconomic development and Westernization. This trend highlights the importance of considering environmental factors in the etiology of the disease.
2. Risk Factors for Ulcerative Colitis
While the exact cause of ulcerative colitis is unknown, several factors are believed to contribute to its development. These include genetic predisposition, environmental factors, and immune system dysregulation.
Genetic Factors
Genetics play a significant role in the development of ulcerative colitis. Individuals with a family history of UC or other inflammatory bowel diseases are at a higher risk of developing the condition. Studies have identified several genetic markers associated with UC, including mutations in the NOD2 gene and other loci involved in immune system regulation. However, genetics alone do not fully explain the occurrence of UC, suggesting that other factors, such as the environment, also play a crucial role.
Environmental Factors
Environmental factors, particularly those associated with urbanization and Westernization, are thought to contribute to the increasing incidence of UC worldwide. Key environmental risk factors include:
- Diet: High consumption of processed foods, red meat, and sugar has been linked to an increased risk of developing UC. In contrast, diets rich in fiber, fruits, and vegetables may have a protective effect.
- Smoking: Unlike Crohn’s disease, smoking appears to have a protective effect against ulcerative colitis. Smokers are less likely to develop UC compared to non-smokers, and individuals who quit smoking may experience an increased risk of UC flare-ups.
- Hygiene Hypothesis: The hygiene hypothesis suggests that reduced exposure to infections and microorganisms in early childhood due to improved sanitation and hygiene practices may contribute to the development of autoimmune diseases like UC. This hypothesis is supported by the higher incidence of UC in more developed countries with high standards of cleanliness.
Immune System Dysregulation
Ulcerative colitis is characterized by an abnormal immune response, where the body’s immune system mistakenly attacks healthy cells in the lining of the colon. This immune dysregulation leads to chronic inflammation and ulceration. Several studies suggest that alterations in gut microbiota, or the balance of bacteria in the digestive system, may play a role in triggering immune responses in UC patients.
3. Demographic Distribution of Ulcerative Colitis
Ulcerative colitis affects individuals across all age groups, genders, and ethnicities, although certain demographic patterns are observed in terms of age of onset, gender, and ethnicity.
Age of Onset
UC typically manifests between the ages of 15 and 30, though it can also occur later in life, with a second peak in incidence observed between the ages of 50 and 70. The early onset of the disease can have significant implications for the patient’s quality of life and long-term management, as UC is a lifelong condition that often requires ongoing medical treatment.
Gender Distribution
In general, ulcerative colitis affects males and females at similar rates. However, some studies suggest a slight male predominance in certain populations. For example, in Western countries, the male-to-female ratio for UC is approximately 1.1:1, whereas in Asian populations, females may be slightly more affected.
Ethnic and Racial Variations
Ethnic and racial differences in the prevalence and incidence of UC have been reported. In the United States, UC is more common among individuals of Caucasian and Ashkenazi Jewish descent compared to African American, Hispanic, and Asian populations. However, recent studies suggest that the incidence of UC is rising in minority populations as well, particularly among African Americans and Hispanics, likely due to changes in environmental and lifestyle factors.
4. Disease Burden and Economic Impact
Ulcerative colitis places a significant burden on healthcare systems and patients worldwide, both in terms of direct medical costs and indirect costs associated with loss of productivity and diminished quality of life.
Direct Medical Costs
The direct medical costs of treating ulcerative colitis include expenses related to hospitalizations, medications, surgeries, and outpatient care. The management of UC often involves long-term use of medications such as 5-aminosalicylic acids (5-ASAs), immunosuppressants, and biologic therapies like anti-TNF agents (e.g., infliximab and adalimumab). These treatments can be costly, particularly for patients requiring advanced therapies or surgery.
In the United States, the annual healthcare cost for UC patients is estimated to be between $8,000 and $15,000 per patient, depending on the severity of the disease. Hospitalizations account for a significant portion of these costs, especially for patients with severe or refractory UC.
Indirect Costs
In addition to direct medical costs, UC imposes indirect costs on patients and society, primarily due to lost productivity and absenteeism. Many individuals with UC experience periods of active disease, or “flare-ups,” which can result in time off work or school and reduced ability to perform daily activities. The unpredictable nature of UC exacerbations also contributes to the emotional and psychological burden of the disease.
Surgical Interventions
Approximately 20-30% of UC patients will eventually require surgery to remove part or all of the colon (colectomy), often due to complications such as severe inflammation, perforation, or cancer risk. While surgery can effectively manage symptoms, it is a major procedure with significant implications for the patient’s long-term health and quality of life. Post-surgical care, including the management of an ileostomy or J-pouch, can also contribute to the overall healthcare burden of UC.
5. Ulcerative Colitis: Future Trends and Challenges
The global burden of ulcerative colitis is expected to continue rising, particularly in developing regions where incidence rates are increasing. This shift will place additional strain on healthcare systems, which may already be under-resourced to manage chronic diseases like UC.
Rising Incidence in Developing Countries
As countries in Asia, the Middle East, and South America undergo rapid industrialization and urbanization, the incidence of UC is expected to increase. Healthcare systems in these regions may face challenges in managing the growing burden of IBD, particularly in terms of access to advanced treatments and specialized care.
Challenges in Disease Management
While advances in biologic therapies have improved the management of UC, several challenges remain. Many patients do not respond adequately to existing treatments, or they may lose responsiveness over time (secondary non-response). Furthermore, biologic treatments can be prohibitively expensive, limiting access for patients in low- and middle-income countries.
There is also a need for more personalized approaches to treatment, as UC is a highly heterogeneous disease. Ongoing research into the role of genetics, microbiota, and immune responses may pave the way for precision medicine in UC, enabling more targeted and effective therapies.
Focus on Early Diagnosis and Prevention
Efforts to improve early diagnosis and prevention of UC complications are essential to reducing the long-term burden of the disease. Increased awareness among healthcare providers and patients, as well as the development of non-invasive diagnostic tools, may help in the early detection and management of UC.
Conclusion
Ulcerative colitis is a complex and chronic disease that poses a significant global health challenge. With rising incidence rates, particularly in developing countries, and the considerable economic burden associated with the disease, it is crucial for healthcare systems to adapt and respond. Advances in treatment options,